tear film assessment test|tear film abnormalities : services This quick, easy assessment of the tear volume on the lower lid shows a good correlation to changes in dry eye. 8 The tear meniscus height indicates whether minimal tear film exists. It also helps us evaluate the quality .
Resultado da 23 de mai. de 2023 · On the official website, Pin Up Casino APK is always updated to the latest version. The distribution has been checked for .
{plog:ftitle_list}
WEB263K Followers, 2 Following, 1,082 Posts - See Instagram photos and videos from Débora Colodro (@deborapattroaofc)
How do you assess for tear film abnormalities? What do the results of these tests tell us about the root cause of dry eye? Why is it important to differentiate aqueous-deficient from evaporative dry eye?Assessment of Tear Film: Tear volume on eye through non-invasive tear meniscus height – slit lamp with or without graticule, tear interference,optical coherence tomography. Tear production through invasive tests - Schirmer .
TBUT serves as an objective measure of tear film stability and can aid in diagnosing and monitoring dry eye disease. It complements other clinical tests for dry eye .Tear film quality should be assessed both with the lens in situ and without the lens. Use of the Tearscope in clinical practice allows a more detailed examination of the tears to be . Schirmer's Test represents a cornerstone in the assessment of tear production, offering insights into the eye's ability to produce both basal and reflex tears. The test involves the strategic placement of a specialized filter . This quick, easy assessment of the tear volume on the lower lid shows a good correlation to changes in dry eye. 8 The tear meniscus height indicates whether minimal tear film exists. It also helps us evaluate the quality .
tear film interferometry
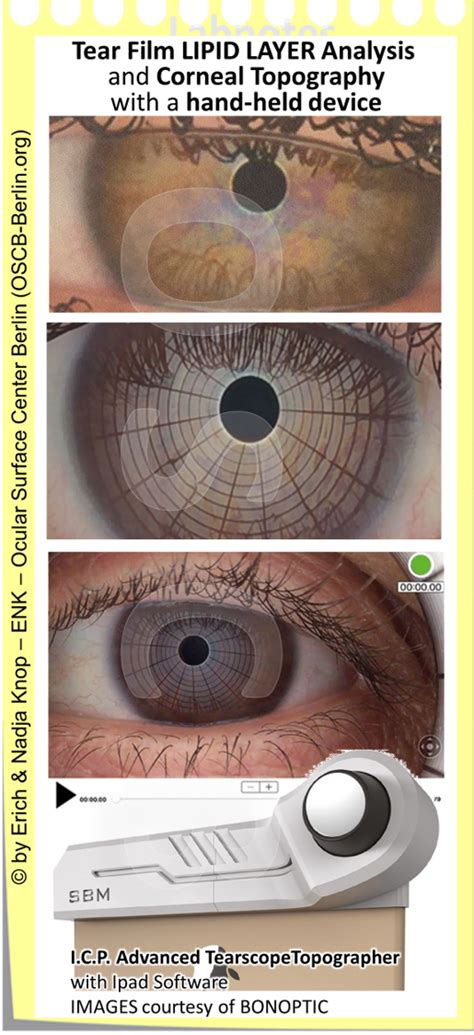
Overview. Dry eye disease (DED) is one of the most frequent conditions in ophthalmology. The early diagnosis and the monitoring of therapy efficacy may help to prevent .
use otc 5610 to test engine compression
Tear break-up time (TBUT), introduced by Norn, 13 remains the most frequently used diagnostic test to determine tear film instability. 14 Generally, the non-invasive tear break .Purpose of review: Dry eye disease (DED) is a complex, multifactorial condition that is challenging to diagnose and monitor clinically. To date, diagnosis has consisted largely of self-reported symptom questionnaires and a collection of clinical tests including vital dye staining, estimation of tear breakup time and Schirmer's testing, as no gold standard exists.
The relation between tear film tests in patients with dry eye disease. Ophthal Physiol Opt. 2003; 23:553–560. doi: 10.1046/j.1475-1313.2003.00153.x. [Google Scholar] 27. Doughty MJ, Whyte J, Li W. The phenol red thread test for lacrimal volume – does it matter if the eyes are open or closed? . Khanal S. Assessment of tear film dynamics . A scientific roundtable on dry eye ranked tear break up time (93%), corneal staining (85%), tear film assessment (76%), conjunctival staining (74%), and the Schirmer test (54%) as the most commonly used diagnostic tests for initial assessment of dry eye. 5 Apart from these traditional clinical tests, we will discuss more about the less invasive .The classically available methods of tear film evaluation are often invasive, with a lack of accuracy and repeatability (Savini et al. 2008). This review attempts to discuss limitations of traditional tear film tests and to highlight advantages and disadvantages of recently introduced non-invasive methods for tear film assessment.
Dr. Monika Soni presented on the topic of tear film at the upgraded department of ophthalmology at MGMMC & MYH Indore. The presentation discussed the anatomy and physiology of tear film, including the three layers of the tear film, mechanisms of tear secretion and distribution, functions of the tear film, tests to evaluate tear film such as tear breakup . Notwithstanding the clinical fortune of fBUT, which became the most common test for tear film assessment 7,8,9, it has been largely recognised for its poor reliability 10,11, (mainly linked to . Various tests to evaluate tear film such as tear film breakup time, Schirmer's test, Rose Bengal staining, and Phenol Red thread test are described. . prior to considering management of any kind In many situations there may be multiple causes and only careful assessment over multiple visits will lead to the correct diagnosis and proper .The test allows the quick assessment of the details of the tear film composition, including the lipid, aqueous and mucin layers, in addition to conjunctival redness classification and MG assessment. The instrument is fit in the slit lamp tonometer hall.
The aim was to determine feasibility and reliability of noninvasive tear break-up time (NIBUT) assessment using handheld lipid layer examination instrument, and to compare it with standard tear break-up time (TBUT) test. Fifty patients were enrolled, 31 with and 19 without dry eye symptoms. Schein q . The time required for the tear film to break up following a blink is called TBUT. It is a quantitative test for measurement of tear film stability. The normal time for tear film break-up is 15–20 s, and abnormal values are generally accepted to be < 10 s using both invasive (with the instillation of fluorescein) and noninvasive techniques . The study aims to assess the tear film before and after phacoemulsification in patients with age-related cataracts. A prospective observational study of 41 age-related cataract patients undergoing phacoemulsification procedure. Tear Film Break-Up Time (TBUT), Tear Film Meniscus Height (TMH), Meibomian glands (MG), and Lipid Layer Thickness (LLT) were .
The first tear film break-up and its location can be seen marked by the 2 red rectangles at 3.5 seconds on the Placido image, as well as a color-coded map with all the break-ups throughout the test, and the time curve of tear film break-up with a first NIBUT at 3.5 seconds and a mean NIBUT of 6.1 seconds.Tear film break-up time is a standard, routine and widely accepted test for tear film stability assessment. It is an invasive method that requires instillation of
Schirmer's (SCH) test and the tear meniscus height (TMH) test measure the quantity of the tear film. Patients diagnosed with aqueous tear deficiency generally have an SCH score of less than 10 mm and a decreased TMH.[4,5,6] Relatedly, the tear film breakup time (TBUT) test measures the quality of the tear film. A rapid TBUT (<10 seconds) is . The fluorescein tear film breakup time (FBUT) measurement is a clinical test that is routinely used to assess the stability of the tear film despite its invasiveness. This test requires the . Rewinding the recordings enabled meticulous assessment of tear film distribution variations over time, minimizing the potential for oversight and enhancing the reliability of TBUT measurements . Purpose: Study the effect on the tear film in blepharospasm (BEB), facial hemispasm (FH), or aberrant regeneration (AR) treated with Botulinum Toxin (BTX-A). Methods: A prospective study was used to evaluate the tear film in patients with BEB, FH, or AR treated with BTX-A. Schirmer tests, break-up time (BUT), optical coherence tomography (OCT) .
Dry eye experts discuss tear film assessment techniques and emphasize the importance of distinguishing between aqueous-deficient and evaporative dry eye for targeted treatment approaches. . Key Diagnostic Tests for Dry Eye Evaluation. Now Viewing. EP: 2.Assessing Tear Film Abnormalities. EP: 3.Need for a Proactive Approach to Dry Eye . A comparison of tear volume (by tear meniscus height and phenol red thread test) and tear fluid osmolality measures in non-lens wearers and in contact lens wearers. Eye Contact Lens 2004 Jul;30(3):132-7. 9. Nichols KK, Nichols JJ, Lynn Mitchell G. The relation between tear film tests in patients with dry eye disease.
Diagnosis of dry eye needs careful assessment of the symptoms along with battery of investigations. . (STT-2, NL-STT2), tear ferning, strip meniscometry test (SMT), tear film breakup time (TFBUT . This test assesses the tear film's stability, as an unstable tear film can trigger reflex tearing. The inferior temporal bulbar conjunctiva is touched with a wet fluorescein staining strip for 1 to 2 seconds. The patient is subsequently asked to blink 2 to 3 times naturally to spread the fluorescein uniformly on the ocular surface. The Tear Film and Ocular Surface Society’s 2017 Dry Eye Workshop II defined dry eye disease (DED) as a multifactorial disease with symptoms of discomfort or visual disturbance, and tear film instability with potential damage to the ocular surface. . tear film osmolarity is an appealing test because it offers a numerical value for dry eye .However, most people with dry eye syndrome/tear film dysfunction have signs of it which are not even obvious on a general, screening eye exam. Depending on the particular constellation of signs, symptoms, history and comorbidities, tests ranging from Schirmer's tear test to blood tests to check for systemic disease may be warranted.
Introduction. The tear film is a thin structure (about 2.0–5.5 µm thick 1, 2), extremely sophisticated in functioning and composition with a crucial role in maintaining ocular surface physiology.The assessment of tear film is of paramount importance in diagnosing dry eye disease (DED) 3, One aspect of the tear film which is crucial to investigate for DED .6.3.1 Current tests 6.3.1.1 Tear film breakup time. In clinical practice, the most frequently employed test of tear film stability is the measurement of the tear film breakup time (TBUT); this is the interval of time that elapses between a complete blink and the appearance of the first break in the tear film [115,116]. 6.3.1.2 Fluorescein .
The diagnostic test of the first choice for the tear film stability assessment, proposed by TFOS DEWS II, is non-invasive tear break-up time (NIBUT) since the instillation of fluorescein during fluorescein tear film break-up time (FBUT) measurement alters the ocular environment [2].The diagnostic test of the first choice for the tear film stability assessment, proposed by TFOS DEWS II, is non-invasive tear break-up time (NIBUT) since the instillation of fluorescein during fluorescein tear film break . Assessment of tear film stability in dry eye with a newly developed keratograph. Cornea. 2013; 32:716-721. Crossref .
Resultado da BIBLIOTECA UniBRASÍLIA; Biblioteca Virtual; Boleto On-line; CPA; Portal do egresso; Periódicos Online; Repositório de TCC; Rematrícula; Contato. .
tear film assessment test|tear film abnormalities